Does insulin really deserve a bad reputation?
 Yes, insulin in excess really does deserve a bad reputation. What follows is Healthy Mind Fit Body’s response to Weightology.net‘s answer to the contrary. Thanks go to blogger/podcaster extraordinaire Jimmy Moore for informing us of this and for reaching out to various other low-carb/Paleo/Primal bloggers to weigh in with their assessments on his Livin’ La Vida Low-Carb blog.
Yes, insulin in excess really does deserve a bad reputation. What follows is Healthy Mind Fit Body’s response to Weightology.net‘s answer to the contrary. Thanks go to blogger/podcaster extraordinaire Jimmy Moore for informing us of this and for reaching out to various other low-carb/Paleo/Primal bloggers to weigh in with their assessments on his Livin’ La Vida Low-Carb blog.
I was fascinated to discover that the author of weightology.net, James Krieger, wrote a post on confirmation bias, apparently around the time he embarked on his five-part series of posts titled “Insulin…an Undeserved Bad Reputation.” Ironically, his post about a common fallacy in thinking and argumentation as well as his five-part series of posts on insulin had a quite familiar ring to them—the one defending the calorie theory of weight loss (“theory” should not be taken in the scientific sense here).
Essentially, Krieger’s posts attempt to challenge the key component in understanding the efficacy of lower carbohydrate/higher fat macronutrient percentages in the human diet to maintain an optimal body fat percentage: the peptide hormone insulin. The insulin factor has been identified as key by a whole host of people, too many in the low-carb/Paleo present (and past) community to mention here. All of us have based our view of insulin on three things: the totality of empirical research on its mechanism of action and systemic effects; an anthropological analysis of the history of food consumption by homo Sapiens; and, the overwhelming benefits of present-day Paleo and various low-carb dietary regimens. So naturally, Krieger has a lot of explaining to do if he seeks to confirm his belief in the status quo calorie theory, which advocates eating fewer calories and exercising more (creating an “energy deficit”) for those who have excess body fat, i.e., are overweight or obese.
Fortunately, as far as insulin being primarily responsible for fat gain and fat storage in humans, we need look no further than James Krieger’s own meta-analysis: Effects of variation in protein and carbohydrate intake on body mass and composition during energy restriction: a meta-regression by Krieger JW, Sitren HS, Daniels MJ, Langkamp-Henken B. After considering a total of 87 studies comprising 165 intervention groups that met the inclusion criteria, the conclusion from this study was the following: “Low-carbohydrate, high-protein diets favorably affect body mass and composition independent of energy intake, which in part supports the proposed metabolic advantage of these diets.” Essentially, subjects lost significantly more fat mass on low-carb regimens than low-fat regimens. Of course, delving into the specifics of those 87 studies referenced is beyond the scope of this article, yet they no doubt provide a pretty thorough perspective on the empirical validity of the insulin factor in weight loss. Many rigorous isocaloric studies support the contention that insulin secretion (via carb consumption) is the primary culprit in fat storage.
Let’s nonetheless explore some of the alleged myths about insulin that Krieger’s posts consider. Unfortunately, variants of the red herring fallacy are particularly evident in the following statements from his first post:
MYTH: Carbohydrate Drives Insulin, Which Drives Fat Storage
FACT: Your Body Can Synthesize and Store Fat Even When Insulin Is Low
Here it seems biochemistry is being turned on its head. There are so many studies indicating that the purported “myth” above is factual that I’m frankly amazed the claim is being made. On the anecdotal side, there are also quite a few individuals who are on ketogenic diets (no carbs) because they are trying to prevent or minimize brain seizures, and this camp is pretty lean. Moreover, any human eating strict Paleo or even the induction phase of the Atkins’ diet doesn’t evidence much fat storage either.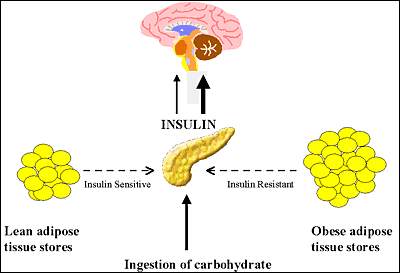
It’s of course true that your body can synthesize and store fat even when insulin is low. But that’s beside the point, because the real question is this: based on empirical analysis, how much fat is synthesized and stored when insulin secretion is low? The answer is of course “very little,” relative to when insulin is high (in terms of daily secretion). This difference is found in the majority of individuals, though by no means all, as I’ll note below.
MYTH: Carbohydrate Is Singularly Responsible for Driving Insulin
FACT: Protein Is a Potent Stimulator of Insulin Too
Well, carbs are primarily responsible for driving insulin secretion. As a type 1 diabetic since 1995, I’m quite familiar with this process. While protein does indeed stimulate your pancreatic beta cells to secrete some insulin (and in my case sometimes requiring an exogenous infusion of insulin), carbohydrates stimulate them more. And as you’ll read below, Krieger himself even concedes this important point.
Now let’s move on to some points made in his second post on insulin,
MYTH: Since diabetics who inject insulin gain weight, this means that insulin is the reason for weight gain in non-diabetics
FACT: Amylin is co-secreted with insulin in non-diabetics; amylin has appetite suppressant and lipolytic effects
Type 1 diabetics are less likely to have overweight issues than type 2 diabetics (having excess body fat increases the likelihood of type 2 diabetes). For most people, body fat gain primarily depends on the amount of carbohydrates being consumed—the more carbs consumed, the more insulin required, and thus the more body fat gained. Any effects of amylin are neglible to this process, and the study that Krieger cites on amylin causing “lipolytic effects” leaves one with more questions than definitive answers. In any event, any fat loss induced by this peptide hormone pales in comparison to what happens when you lower your insulin levels.
MYTH: Lowering Insulin Will Improve Appetite Regulation
FACT: Insulin Is One of the Many Hormones Critical to Satiety
Individuals suffering from hyperinsulinemia might beg to differ on this one. Satiety is a complex issue, to be sure, and insulin’s role here is no exception. If anything, the evidence shows the opposite of the “fact” above; higher insulin secretion will tend to promote more consumption of carbs, reflecting the proverbial sweet tooth or junk food junkie behaviors. Whether this is a psychological or physical phenomenon or a combination of both is difficult to ascertain. Whether people consume high-carb/low fat foods or low-carb/high fat foods has a lot to do with their knowledge and their motivation too.
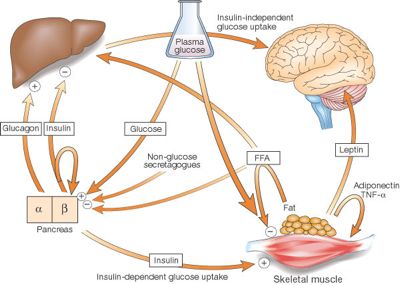 And as we noted on our podcast (episodes 58 and 59), if insulin works on the brain to cause a feeling of satiety, and insulin resistant individuals do not respond as effectively to some of the effects of insulin, it is possible that some individuals may be resistant to the satiety-promoting effects of insulin—causing them to feel hungry despite high insulin levels. Leptin, another hormone which has been shown to promote satiety in healthy individuals, is found at unusually high levels in obese people, but they still feel hungry. Leptin resistance may be to blame. Dozens of other hormones affect appetite in some way, and the overall feeling of satiety or hunger is probably a net result of many different hormones.
And as we noted on our podcast (episodes 58 and 59), if insulin works on the brain to cause a feeling of satiety, and insulin resistant individuals do not respond as effectively to some of the effects of insulin, it is possible that some individuals may be resistant to the satiety-promoting effects of insulin—causing them to feel hungry despite high insulin levels. Leptin, another hormone which has been shown to promote satiety in healthy individuals, is found at unusually high levels in obese people, but they still feel hungry. Leptin resistance may be to blame. Dozens of other hormones affect appetite in some way, and the overall feeling of satiety or hunger is probably a net result of many different hormones.
So, how important is the contribution of insulin to feelings of satiety and hunger, compared to other hormones? That question does not have a definitive answer. Again, it is complicated and difficult to study the role that any individual hormone plays in regulating hunger, but insulin does not represent the entire picture.
The second post on insulin by Krieger concludes with the following statement:
As I mentioned earlier, people seem to confuse blood glucose control and insulin control. It is the management of blood glucose itself that is partly responsible for the health benefits of low-glycemic carbohydrates, or reducing carbohydrates, or increasing protein intake, or consuming dietary fiber, or consuming fruits and vegetables, or consuming whole foods over processed foods. It is not the control of insulin; the control of insulin ends up being a byproduct of these other behaviors through improvements in insulin sensitivity (how responsive your cells are to insulin) and reductions in blood sugar swings.
This explanation misses the mark, as demonstrated by my own experience of taking tens of thousands of blood glucose readings over the last 16 years, since I was diagnosed with type 1 diabetes. As I noted on our podcast, my blood glucose levels tend to fluctuate a lot more than non-diabetics’ levels do, because 1) injecting insulin subcutaneously doesn’t have as immediate an effect as when it’s secreted endogenously by your pancreas (though I still do secrete some insulin endogenously) and 2) the regular insulin I inject in bolus amounts for meals doesn’t exactly match the digestion and conversion of carbs to glucose into the bloodstream and thus the exact demand for insulin, in order to keep blood glucose in the normal range (say, 80-120 mg/dL). (On average, however, my A1c (glycated hemoglobin) levels are typically 5-6%, which should forestall many of the long-term complications such as retinopathy, neuropathy, and nephropathy.)
Yet, I’m nevertheless at my ideal weight with about 10% body fat, which I’ve maintained for years, ever since I began a reduced carb/increased fat diet in 1997 (losing five percentage points in body fat in the process). It’s clear, not only from my personal experience as my own best doctor and patient but also by a plethora of studies, that total amount of insulin secretion is the primary factor in body fat level—particularly in the majority of the human population with a genotype that tends to store carbs as fat rather than burn them. For the segment of the human population who can eat lots of carbs without gaining fat, this is arguably an even less fortunate phenomenon, because it may lead to the unwarranted assumption that their higher level of insulin secretion is healthy (“I’m not overweight, so I’m healthy!”).
At the end of Part 3 on insulin, Krieger offers an explanation as to why he’s not fat:
Why Am I Not Fat?
My own personal experience with dairy fits right in with the science. I consume a lot of dairy and have for many years. I go through 2-3 gallons of milk per week. I also go through a lot of Greek yogurt, cottage cheese, regular cheese, and whey protein. I have some type of dairy with just about every meal. Thus, I have large amounts of insulin flowing through my body pretty much all day. If insulin was truly the fat-promoting, weight-gaining hormone that some have made it out to be, then I should be obese by now. Yet, I am not …not even close.
Not only that, but the people who think insulin makes you hungry, that would imply that I should be starving all of the time with all of the insulin that is flowing through my body all day. Yet, Im not.
Got Milk? Got Insulin!
The evidence is overwhelming that dairy products do not promote weight gain, and they actually inhibit weight gain in animal studies. This is despite the fact that dairy products produce very large insulin responses, as much or greater than many high carbohydrate foods. Thus, it is clear from this article, as well as my previous articles, that the carbohydrate/insulin hypothesis is incorrect. Insulin is not the criminal in the obesity epidemic; instead, it is an innocent bystander that has been wrongly accused through guilt by association.
Just because he has not accumulated excess body fat as a result of the various carbs in his dairy product consumption doesn’t mean that others experience similar results. In fact most people who consume excess carbs, whether in the form of milk or cookies, will store more body fat than, say, if they were eating cheese and whey protein. To his point, I have experienced a slightly higher requirement of insulin when consuming whey protein powder and even yogurt (I eat the healthier whole-fat kind), but it’s not nearly as pronounced as when I consume extra bread or a banana, for instance.
Thus, it’s important not to treat all dairy as identical in terms of the insulin factor. For instance, I stopped drinking milk about a decade ago, in order to reduce my total daily carb consumption, and I lost body fat and my blood lipids (HDL and triglycerides) improved. Cheese requires very little insulin, unless you venture into the realm of the carb-containing processed Velveeta and cheese slices.
In the fourth post on insulin, which was one of particular interest to me (being a type 1), we encounter some more claims that constitute red hearing fallacies:
Insulin Is Not Required for Cells To Take Up Glucose […and…] Glucose Transport is Not Insulin Dependent
While it’s true that some glucose is uptaken via cell membrane channels other than GLUT-4, which is the channel responsive to the insulin receptor, this is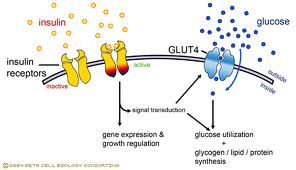 irrelevant because most glucose uptake (i.e., by cells responsive to insulin, about 40% in a fasting, resting state) does require insulin.
irrelevant because most glucose uptake (i.e., by cells responsive to insulin, about 40% in a fasting, resting state) does require insulin.
The two studies that Krieger references are interesting, in that they focus on insulin’s inhibitory action on glycogenolysis and gluconeogenesis by the liver, but they fail to prove his claim that insulin isn’t the key aspect of fat storage. Sure, basal insulin levels keep the liver from adding excess glucose into your bloodstream, but what matters is the insulin secreted to deal with the carbs that you consume (the bolus insulin amounts). For instance, of the typical 30 units of insulin I inject per day, at least 20 units are used to deal with the typical 100 grams of carbs I consume per day; thus, most of the insulin injected is dedicated to glucose uptake into my lean tissue and fat tissue.
In a summation of this fourth post, Krieger wrote:
When you inject insulin into an uncontrolled diabetic, you are now providing a brake on all of the processes mentioned earlier. You inhibit production of glucose by the liver, so blood sugar falls. Because there is no longer hyperglycemia, glucose uptake into cells actually decreases. Lipolysis is inhibited, so free fatty acid concentration falls to near zero. Because there are no longer free fatty acids to make ketones, ketone production slows down. Proteolysis is also inhibited.
Insulin does indeed inhibit production of glucose by the liver, which causes blood glucose to either remain at a current level or fall; it all depends on how much insulin is injected. A basal rate amount of insulin will not typically cause blood glucose to fall, but rather remain homeostatic (unless affected by intense exercise, which can act as an “invisible insulin”). When a bolus amount of insulin is injected so that a meal with carbs can be consumed, blood glucose will either stay the same, lower, or even increase (due to either the misalignment of timing of the peak insulin and carb digestion periods, or not injecting enough insulin to deal with the carb amount).
Explaining insulin’s function in a fasting type 1 diabetic doesn’t enable us to determine insulin’s function during a meal state. Advocates of low-carb diets of course concur that insulin inhibits lypolysis (and proteolysis and ketone production), for this is the central reason why people who eat more carbs typically have a much harder time burning their own body fat.
More from Krieger’s fourth-post summary:
Insulin – More of a Traffic Cop Than a Storage Hormone
Metabolic tracer studies have proven what Schafer had hypothesized nearly a century ago …that insulin’s main role in the body is inhibitory rather than excitatory. While insulin certainly does have excitatory functions, it is not primarily a storage hormone that many individuals claim that it is. Insulin is not needed for your cells to take up and store glucose. Certainly, it enhances uptake, but there is a big difference between enhancing uptake and being needed for uptake.
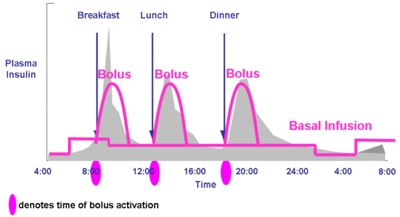 The above claims are not only unsubstantiated, but also yet another red herring fallacy. If you read in detail the study that Krieger relies on to make this claim, and the other study he references (done by one of the same researchers 22 years later, mind you), you’ll find that mixed in with many basic truths about insulin and metabolism, are a lot of false claims regarding the main role of insulin. Again, as any type 1 diabetic who uses an insulin pump (and their attending physician) will tell you, basal insulin rate amount is much less than the total of daily bolus infusions. In other words the amount of insulin required on a daily basis to prevent your liver from adding glucose to your bloodstream (via glycogenolysis or gluconeogenesis) is significantly less than the amount of insulin necessary to induce the uptake of glucose into your fat, muscle, and other lean tissue cells, created by the carbs you consume during your meals.
The above claims are not only unsubstantiated, but also yet another red herring fallacy. If you read in detail the study that Krieger relies on to make this claim, and the other study he references (done by one of the same researchers 22 years later, mind you), you’ll find that mixed in with many basic truths about insulin and metabolism, are a lot of false claims regarding the main role of insulin. Again, as any type 1 diabetic who uses an insulin pump (and their attending physician) will tell you, basal insulin rate amount is much less than the total of daily bolus infusions. In other words the amount of insulin required on a daily basis to prevent your liver from adding glucose to your bloodstream (via glycogenolysis or gluconeogenesis) is significantly less than the amount of insulin necessary to induce the uptake of glucose into your fat, muscle, and other lean tissue cells, created by the carbs you consume during your meals.
Insulin is needed for uptake of glucose into cells during meals; insulin doesn’t merely “enhance” uptake. Of course, we should keep in mind that during a fasting, resting state, roughly 60% of glucose in your bloodstream is being used by cells that don’t require insulin, namely the brain and other nerve cells and red blood cells. The percentage of uptake of glucose by various tissues of course changes dramatically as soon as you start moving around and eating things.
In his finale post, Krieger lists his reasons for why insulin allegedly is not the main culprit in people with weight issues:
The ‘carbohydrates drive insulin which drives fat storage’ mantra is a perfect example of cognitive miserliness. It is a concept that is based on incomplete information regarding insulin, carbohydrate, and body weight regulation. Many people are drawn to this hypothesis because of its simplicity. However, its simplicity is exactly what makes it incorrect, because it does not address all the available data. It is a shortcut in thinking, based on a narrow view of insulin’s effects on lipolysis and glucose.
Well, given what we’ve explored so far, an appropriate retort to the above is simply, “Saying it doesn’t make it so.” Though we addressed on our podcast some main points on his list of reasons for not impugning insulin (episodes 58 and 59), let’s address some final ones here:
Very high carbohydrate diets have been demonstrated to produce weight loss when people are in an energy deficit
This is true, but it’s overlooking the overwhelming amount of evidence (including Krieger’s own meta-analysis) that very low carb diets have induced significantly more body fat loss in individuals than very high carb diets. And as Atkins noted, the ultimate “energy deficit” diet—starvation, or fasting—doesn’t burn as much body fat as the “fat fast” diet, consisting of a thousand calories per day, 90% fat and 10% protein, which has been demonstrated to shed body fat the fastest. In other words the calorie theory of weight loss is overly simplistic, because it doesn’t take into account the huge metabolic effects of the hormone insulin.
A type I diabetic without insulin becomes hyperglycemic because of overproduction of glucose by the liver, not because insulin can’t get into cells
Once again, this is not taking into account all the evidence. Sure, in a fasting state the liver does cause hyperglycemia (i.e., for those diabetics with not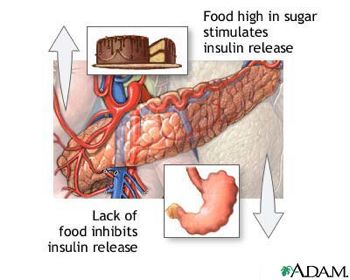 enough beta cells still functioning; my own cells are able to handle the amount of glucose output from my liver in a fasting state—two years ago I fasted for 4 days and my blood glucose readings were normal, despite injecting no insulin). Additionally, when hyperglycemia occurs in a fasting state for type 1s, if glucose could enter our fat and lean tissue cells without insulin, it would result in normal blood glucose levels. So, even though the cause of high blood glucose in a fasting state is the liver’s production of glucose, the other half of the story is that this hyperglycemia would not occur if none of our cells required insulin to clear glucose from our bloodstream.
enough beta cells still functioning; my own cells are able to handle the amount of glucose output from my liver in a fasting state—two years ago I fasted for 4 days and my blood glucose readings were normal, despite injecting no insulin). Additionally, when hyperglycemia occurs in a fasting state for type 1s, if glucose could enter our fat and lean tissue cells without insulin, it would result in normal blood glucose levels. So, even though the cause of high blood glucose in a fasting state is the liver’s production of glucose, the other half of the story is that this hyperglycemia would not occur if none of our cells required insulin to clear glucose from our bloodstream.
You cannot simply look at the temporary effects of insulin on lipolysis and glucose storage. You have to address what is happening over a 24-hour period; body fat will not increase if there is no overall energy surplus.
Dont be a cognitive miser. Insulin is not the bad guy.
To the contrary, insulin is indeed a bad guy, and there’s no compelling reason to support the non-hormonal calorie myth of weight gain/loss; it’s an unscientifically simplistic notion that basically floats the mainstream nutritional boat. Still, Krieger noted the following in his Part 5 post (Addressing the Critics),
Therefore, it comes down to a matter of energy balance. The postprandial insulin secretion is irrelevant…insulin cannot trump the laws of physics.
Thus, we’ve come full circle. The conclusion drawn from his meta-analysis mentioned at the beginning of this critique contradicts his above claim. The energy surplus/deficit notion (aka the calorie theory) of weight loss is misguided at best when one factors in the hormonal side of metabolism—as one astute researcher wrote, “We have got the first principle of dieting wrong. Energy in does not equal energy out (put a gallon of petrol in a diesel car if you question this).”
Let’s conclude with a few more statements from Krieger’s post 5,
Certainly, when you average across all foods, carbohydrate produces the greatest insulin responses, and protein comes in second. However, when you start looking at individual foods, some protein sources can produce similar insulin responses to some carbohydrate foods (even some carbohydrate foods that create rapid rises in blood glucose). And this is not to mention the synergistic effect that protein and carbohydrate can have on insulin secretion when consumed together. Yet, studies that have combined the two have shown large amounts of weight and fat loss.
“Large amounts of weight and fat loss” as a result of combining consumption of carbs and protein compared to what, and under what conditions? There are a lot of questions being begged by the above claims, in addition to much research being overlooked. Moreover, there is no mention of fat in the fat-loss equation.
However, the vast majority of prospective studies have failed to show a relationship between either basal or postprandial insulin levels and future weight gain; in fact, some studies have shown higher insulin levels to be predictive of less weight gain in overweight people. Also, insulin levels are not predictive of weight loss.
Thus, the concept that high insulin drives fat storage is a concept not supported by the scientific data.
 Wow, case closed, right? Not hardly. In fact, just the opposite. Writing such inaccurate statements does not make them magically come true. In the studies included in Krieger’s own meta-analysis, study participants who were followed over 12 weeks or more, and who ate a low-carb diet, lost 14 lbs of body weight more than low-fat dieters. When comparing loss of body fat between those eating low-carb and low-fat diets, low-carb eaters lost 12 lbs more fat mass than the low fat group. As in all things, it’s important to separate one’s observations of the empirical research from one’s evaluations of it; it’s important to draw sound conclusions. People have needs for understanding and objectivity in these matters, so that they can regain and maintain optimal health and well-being.
Wow, case closed, right? Not hardly. In fact, just the opposite. Writing such inaccurate statements does not make them magically come true. In the studies included in Krieger’s own meta-analysis, study participants who were followed over 12 weeks or more, and who ate a low-carb diet, lost 14 lbs of body weight more than low-fat dieters. When comparing loss of body fat between those eating low-carb and low-fat diets, low-carb eaters lost 12 lbs more fat mass than the low fat group. As in all things, it’s important to separate one’s observations of the empirical research from one’s evaluations of it; it’s important to draw sound conclusions. People have needs for understanding and objectivity in these matters, so that they can regain and maintain optimal health and well-being.
Best wishes to those on this journey!
Wes
2 thoughts on “Does insulin really deserve a bad reputation?”